Insights:
Vasculitides can be characterised by hypersensitivity reactions: type 1 (Churg-Strauss), type 2 (Kawasaki), type 3 (polyarteritis nodosa) and type 4 (granulomatosis with polyangiitis).
Endothelial dysfunction can lead to a hypercoagulable state, endothelial hyperplasia narrows the lumen- these increase risk of thromboembolism. Medial degeneration can lead to loss of elasticity and aneurysms. Adventitial fibrosis can stiffen the artery. In general there is a pro-inflammatory state in the vessels, with neutrophil, monocyte and lymphocytic infiltrate with or without complement.
Some vasculitides are pauci-immune (i.e. no immune complex or complement activation). These have anti-neutrophil cytoplasmic antibodies. Interestingly, the mechanism behind agranulocytosis in the treatment of hyperthyroidism with PTU is formation of ANCAs that trigger lysis of granulocytes (Akamizu et al., 2002).
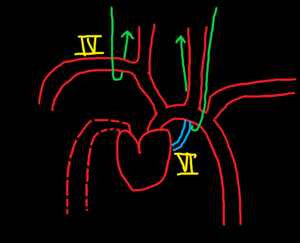
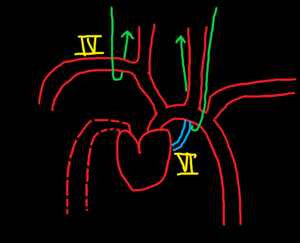
The clinical picture depends largely on which vessels are affected. Common to all are systemic features of fatigue, weight loss and malaise.
References
Kumar, V. (2017). Robbins basic pathology international edition. [S.l.]: Elsevier - Health Science.
Akamizu, T., Ozaki, S., Hiratani, H., Uesugi, H., Sobajima, J., Hataya, Y., Kanamoto, N., Saijo, M., Hattori, Y., Moriyama, K., Ohmori, K. and Nakao, K. (2002). Drug-induced neutropenia associated with anti-neutrophil cytoplasmic antibodies (ANCA): possible involvement of complement in granulocyte cytotoxicity. Clinical & Experimental Immunology, 127(1), pp.92-98.




 View all episodes
View all episodes


 By Damian Amendra
By Damian Amendra